Retina San Diego is home to the most advanced technology in the treatment of diabetic retinopathy.
WHAT IS DIABETES MELLITUS?
Diabetes is a chronic disease in which our body does not regulate blood sugars sufficiently. It most commonly happens in older patients (type 2 Diabetes) who develop a resistance to the substance that regulates blood sugar, called insulin. It can also affect younger patients (type 1 diabetes) who have difficulties producing insulin.
29.1 million people in the U.S. have diabetes, of which 8.1 million are undiagnosed. The eye doctor in a lot of cases can be the first person who sees signs of diabetes.
High levels of blood sugar can damage the blood vessel walls throughout the body, and with time cause significant damage to all your organs. Uncontrolled diabetes can affect your vision, the sensation in your toes thus increasing your risk for infection, your kidneys, your heart, and your brain. People with uncontrolled chronic diabetes have a higher chance of getting bleeding in their eyes that can be sight-threatening, and have a higher chance of heart attacks or strokes.
WHAT IS DIABETIC RETINOPATHY?
Diabetic retinopathy is the number one cause of blindness in working-age Americans today. High levels of blood sugar cause damage to the small blood vessels in the body called capillaries. Patients with diabetes lose some of the cells critical to the health of the blood vessels. The absence of these cells, called pericytes, causes the blood vessel wall to become leaky and allow some of the fluid within your blood to leak into the retina, thus affecting the function and the health of the cells within the retina that are in charge of your vision.
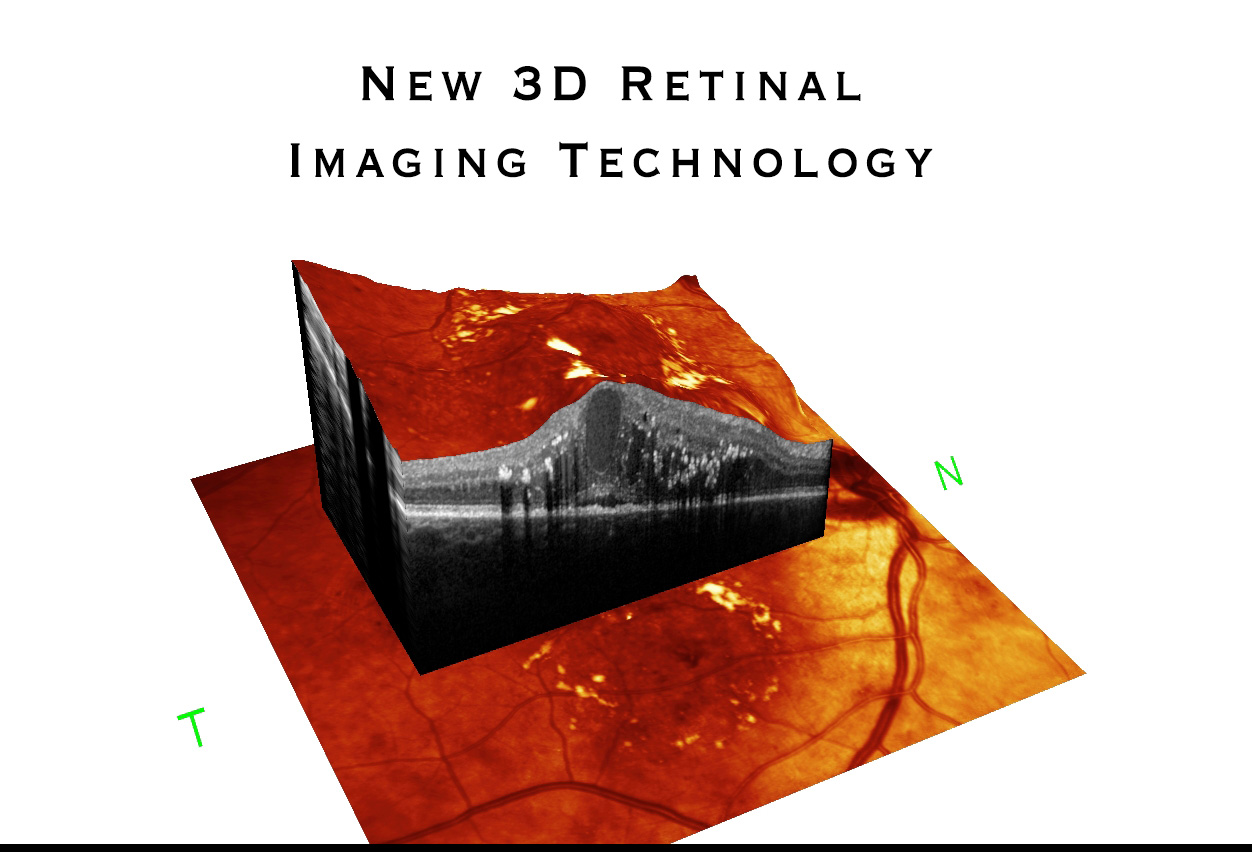
The leakage within the retina causes a swelling of the central part of the retina called the macula which is in charge of your central and most acute vision. Diabetic macular edema (edema = swelling), i.e. "swellling of the central part of the retina" affects one million Americans and should be evaluated and treated before irreversible damage has occurred to the retina.
In advanced cases where the blood flow is critically diminished within the eye, the body reacts by creating abnormal blood vessels (a stage of disease called Proliferative Diabetic Retinopathy) which unfortunately can bleed within the eye (called Vitreous Hemorrhage) or lead to scar tissue formation that can cause retinal detachments and significantly affect vision.
WHAT CAN I DO TO PREVENT VISION LOSS?
Prevention is always the most effective treatment in medicine, and in diabetes it consists of keeping your blood sugar controlled. This requires a close follow up with your medical doctor to make sure you have the correct medicine and its appropriate dosage. A healthy diet along with regular cardiovascular exercise and routine blood sugar monitoring are critical. Blood sugar should be routinely tested at home with your personal blood sugar monitoring machine and can be tested every 3 months by your doctor by checking your blood's "Hemoglobin A1c". This blood test provides an average of your blood sugar level for the last 3 months. We recommend that you write down and memorize your number so you can follow your progress.
Blood pressure control and monitoring your cholesterol levels are important as they can contribute to the damage that can happen to your blood vessels.
WHAT IS THE TREATMENT FOR DIABETIC MACULAR EDEMA AND PROLIFERATIVE DIABETIC RETINOPATHY?
The last decade saw the advent of a new family of medications used in the treatment of diabetic macular edema (DME) and proliferative diabetic retinopathy (PDR), called anti-VEGF drugs.Vascular Endothelial Growth Factor (VEGF) is a substance produced within the body that causes the growth of new blood vessels and plays a role in the permeability of the blood vessel walls. Patients with diabetic retinopathy have leaky blood vessels and higher levels of VEGF within their eyes that can cause the growth of abnormal leaky blood vessels on the retina (called neovascularization) which can bleed and significantly affect vision. Anti-VEGF drugs inhibit the abnormally high levels of VEGF within the eye and thus cause regression of some of these blood vessels or cause stabilization of the blood vessel wall which decreases the swelling (edema) within the retina, thus improving vision.
The medication is given with a very small needle after proper anesthesia has been administered to the eye, and the vast majority of patients report little or no discomfort with the treatment. The medication lasts about 1 month and may be required as continued therapy. Your retina specialist will start you on a series of injection therapy sessions and will attempt to increase the interval between injections.
What are the 3 medications used?
Lucentis (ranibizumab): First anti-VEGF drug to be approved for intraocular use for diabetic macular edema and proliferative diabetic retinopathy. Because of its smaller molecule, Lucentis has the least effect on systemic VEGF levels and is cleared faster from the system compared to the other anti-VEGF drugs.
Avastin (bevacizumab): Avastin was developed by the same company as Lucentis however it was approved for certain cancer treatments, but has since then been found to be effective and safe for treatment of diabetic macular edema and proliferative diabetic retinopathy. It is the drug that is most often used in the U.S. mainly because of its lower cost.
Eylea (aflibercept): Eylea is FDA approved for treatment of wet AMD and has a stronger affinity to VEGF. Eylea can be more beneficial than its counterparts in the treatment of diabetic patients with the worst vision at baseline.
HOW CAN THE NEW YELLOW LASER BENEFIT ME?
Retina San Diego is the first center in San Diego to have brought the new YELLOW LASER MICROPULSE technology to our community. This new laser allows us to treat patients with diabetic macular edema that has affected the center of their vision without causing a scar like older LASERs would. It is more gentle to the retina and is a great adjunct to intravitreal anti-VEGF therapy in select patients.
WHAT IS THE TREATMENT FOR DIABETIC TRACTIONAL RETINAL DETACHMENT?
In advanced stages, proliferative diabetic retinopathy can lead to scarring on the retina which can contract and elevate the retina thus causing what is called a tractional retinal detachment (TRD) which can affect the vision. TRD can be observed if they are small and not affecting vision, however if they are noted to increase in size or affect central vision, the fibrotic scar on the retina should be removed in order to allow the retina to flatten and regain some function.